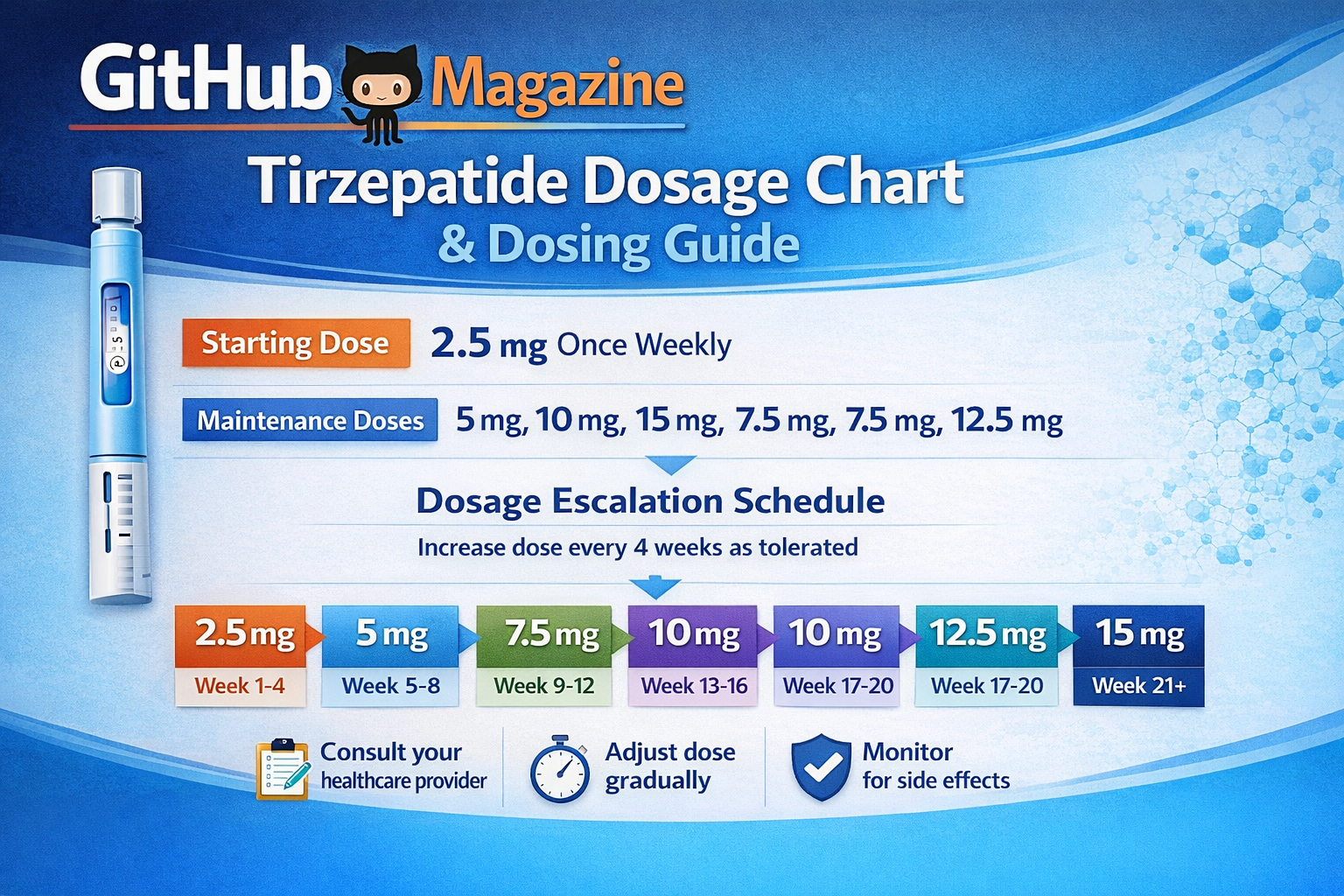
Tirzepatide Dosage Chart Explained
Tirzepatide has become one of the most discussed injectable medicines in metabolic care, reshaping how clinicians approach type 2 diabetes and chronic weight management. Readers searching for a “tirzepatide dosage chart” are usually looking for something simple: how much to take, when to increase the dose, and what the safe upper limits are. The short answer is that tirzepatide is not started at its strongest dose. Instead, it follows a carefully structured weekly schedule that begins low, rises gradually, and stabilizes at a personalized maintenance level designed to balance results with tolerability.
In its approved formulations, tirzepatide is taken once a week as a subcutaneous injection. Treatment almost always begins at 2.5 milligrams weekly, a dose chosen not for maximum therapeutic effect but to help the body adjust. After four weeks, most patients move to 5 milligrams, and then—if needed—progress in 2.5-milligram steps every four weeks. The maximum recommended dose is 15 milligrams once weekly. Some patients never need to reach that level. Others do, particularly when weight loss or more intensive glucose control is the goal.
Behind this schedule lies the drug’s dual mechanism of action on GIP and GLP-1 receptors, hormones involved in insulin secretion, appetite regulation, and digestion. These same pathways that drive clinical benefits also explain why nausea, fullness, and other gastrointestinal symptoms can occur when doses rise too quickly. The dosage chart exists, in effect, to protect patients from their own progress.
For Git-Hub Magazine’s health and science readership, this article brings together the established dosing structure, real-world clinical practice, and safety principles into a single reference guide. It is written to be practical, current, and grounded in how tirzepatide is actually prescribed today.
How Tirzepatide Dosing Is Designed
Tirzepatide dosing is built around a principle known as titration. Rather than prescribing a fixed amount for every patient, clinicians adjust the dose upward in stages, allowing time for the body to adapt. This approach reflects both pharmacology and experience from large clinical trials, where slower dose increases were linked to fewer discontinuations and better long-term adherence.
The medication is administered once weekly, on the same day each week when possible. It can be injected into the abdomen, thigh, or upper arm, and injection sites are rotated to avoid irritation. The weekly rhythm is central to its design: steady drug exposure, gradual accumulation, and predictable response.
The starting dose of 2.5 milligrams is considered introductory. It is not intended to deliver full glucose-lowering or weight-loss effects. Instead, it prepares the digestive system and central appetite pathways for stronger stimulation later. After four weeks, clinicians typically increase the dose to 5 milligrams, which is the first level at which most patients begin to notice meaningful metabolic changes.
Further increases are optional and individualized. Some patients achieve excellent control at 5 or 7.5 milligrams. Others require higher doses to reach their clinical targets. The structure is flexible but bounded by a maximum of 15 milligrams weekly, the highest dose evaluated and approved in regulatory trials.
Standard Tirzepatide Dosage Chart
The following table summarizes the commonly used escalation pathway in adult patients.
| Treatment period | Weekly dose (mg) | Clinical purpose |
|---|---|---|
| Weeks 1–4 | 2.5 | Initiation and tolerance building |
| Weeks 5–8 | 5.0 | First therapeutic dose |
| Weeks 9–12 | 7.5 | Optional escalation |
| Weeks 13–16 | 10.0 | Advanced therapeutic range |
| Weeks 17–20 | 12.5 | Further escalation if needed |
| Week 21 onward | 15.0 | Maximum maintenance dose |
This chart reflects a typical progression rather than a mandatory path. Patients may remain at a lower dose for extended periods or stop escalating once clinical goals are met. In everyday practice, the “best dose” is the lowest dose that provides sufficient benefit with acceptable side effects.
Dosing by Indication: Diabetes and Weight Management
Although the dosing structure is similar across indications, treatment goals differ. For diabetes, the primary aim is glycemic control. For obesity, the aim is sustained weight reduction and improvement of metabolic risk factors. These differences influence how aggressively clinicians pursue higher doses.
| Indication | Starting dose | Common maintenance doses | Maximum dose | Practical notes |
|---|---|---|---|---|
| Type 2 diabetes | 2.5 mg weekly | 5–10 mg | 15 mg | Adjusted to reach HbA1c targets |
| Chronic weight management | 2.5 mg weekly | 10–15 mg | 15 mg | Higher doses often used for appetite suppression |
| Sleep apnea related to obesity | 2.5 mg weekly | 10–15 mg | 15 mg | Weight loss is the therapeutic driver |
In diabetes care, many patients stabilize at moderate doses because glucose targets are reached earlier. In weight management, higher doses are more common, reflecting the dose-dependent effect on appetite and satiety.
Timing, Missed Doses, and Practical Use
Consistency matters more than precision to the hour. Tirzepatide should be taken on the same day each week, but the exact time of day is flexible. If a patient misses a dose, it can be taken within four days of the scheduled time. If more than four days have passed, the missed dose is skipped and the next injection is taken on the regular schedule.
This rule exists to prevent overlapping doses that could intensify side effects. Because tirzepatide has a long half-life, stacking injections too closely together can significantly increase nausea or vomiting.
Clinicians often advise patients to pair their injection day with a routine event, such as a weekend morning or a workday evening, and to use reminders. The goal is not just correct dosing but sustained adherence over months and years.
Why Slow Escalation Matters
Gastrointestinal side effects are the most common reason patients discontinue tirzepatide. Nausea, bloating, early fullness, and diarrhea tend to appear when doses rise faster than the body can adapt.
An endocrinologist quoted in clinical dosing guidance summarizes the reasoning clearly: starting low and increasing gradually “allows the gut and appetite centers in the brain to recalibrate without overwhelming the patient.”
A pharmacology review in prescribing literature echoes this view, noting that therapeutic benefit correlates more strongly with maintaining a tolerable dose than with reaching the highest possible dose.
A third expert perspective from metabolic specialists emphasizes personalization. Patients differ in how sensitive they are to GLP-1 and GIP stimulation. For some, 7.5 milligrams is transformative. For others, it barely registers. The dosage chart is therefore a framework, not a mandate.
Safety Considerations in Dose Selection
Tirzepatide does not usually require dose adjustment for age, mild kidney disease, or mild liver disease. However, clinicians are cautious in patients prone to dehydration or with a history of severe gastrointestinal reactions.
Dose escalation may be delayed or paused if side effects interfere with daily life or nutrition. In rare cases, patients reduce their dose after escalation if symptoms persist. This is considered acceptable practice when balanced against therapeutic goals.
Another safety factor is concurrent medication. Patients using insulin or sulfonylureas may need adjustments to those drugs as tirzepatide doses rise, to avoid hypoglycemia.
How Clinicians Decide on a Maintenance Dose
Maintenance dosing is where science meets judgment. Laboratory results, weight trends, patient feedback, and side-effect profiles all influence decisions.
For diabetes, clinicians look primarily at HbA1c levels and fasting glucose. For weight management, percentage weight loss over three to six months often guides whether escalation continues. Many specialists aim for a maintenance dose that produces steady improvement without daily discomfort.
In long-term studies, a significant proportion of patients remained on 10 or 15 milligrams, but a substantial minority achieved durable benefits at lower doses. This diversity is why no single number defines success.
The Dosage Chart in Real-World Care
In textbooks, dosing charts look linear and tidy. In practice, they are more fluid.
A patient might spend two months at 5 milligrams because nausea persists, then move directly to 10 milligrams once symptoms resolve. Another might advance step by step but decide to stop at 12.5 milligrams because weight loss plateaus but quality of life remains high.
The chart is therefore best understood as a map rather than a timetable. It shows what is possible, not what is mandatory.
Takeaways
- Tirzepatide is started at 2.5 mg weekly to build tolerance.
- Dose increases usually occur every four weeks in 2.5 mg steps.
- The maximum approved dose is 15 mg once weekly.
- Many patients achieve good results at lower doses.
- Weight management often requires higher maintenance doses than diabetes control.
- Missed doses can be taken within four days, otherwise skipped.
Conclusion
The appeal of tirzepatide lies not only in its clinical power but in the careful architecture of its dosing. The gradual climb from 2.5 to 15 milligrams reflects decades of lessons from metabolic medicine: rapid results mean little if patients cannot stay on therapy. The dosage chart is therefore as much about patience as potency.
For readers of Git-Hub Magazine, accustomed to systems thinking in technology and engineering, tirzepatide’s design may feel familiar. It is a modular process, built on incremental upgrades, constant monitoring, and adaptive optimization. Each dose is a version release, tested in the environment of an individual human body.
Understanding this structure helps patients set realistic expectations and clinicians make informed adjustments. The chart does not promise instant transformation. It promises something more durable: a pathway toward metabolic stability, taken one week at a time.
FAQs
What is the usual starting dose of tirzepatide?
2.5 milligrams once weekly, primarily to build tolerance.
How often is the dose increased?
Typically every four weeks, depending on side effects and response.
What is the highest approved dose?
15 milligrams once weekly.
Can I stay on a lower dose long-term?
Yes. Many patients maintain good results at 5, 7.5, or 10 milligrams.
What happens if I miss an injection?
Take it within four days if possible; otherwise skip and resume the next week